Mitigation can buy us time, but only suppression can get us to where we need to be.
MARCH 19, 2020
Professor of pediatrics at Indiana University School of Medicine
Professor of Global Health at Harvard University
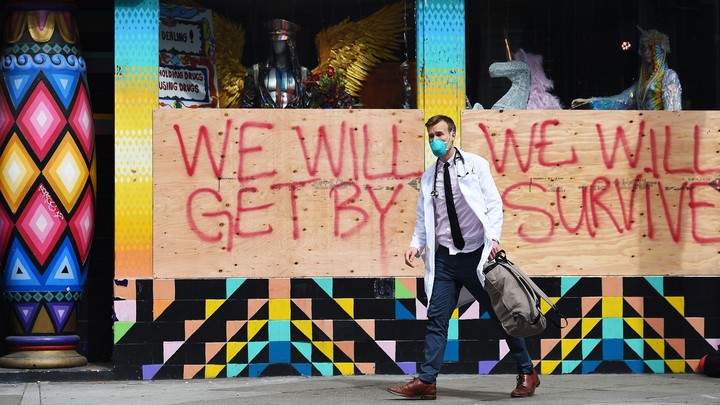
JOSH EDELSON / AFP / GETTY
While many watched the coronavirus spread across the
globe with disinterest for months, in the last week, most of us have finally
realized it will disrupt our way of life. A recent analysis from Imperial College is now
making some Americans, including many experts, panic. The report
projects that 2.2 million people could die in the United
States. But the analysis also provides reason for hope—suggesting a path
forward to avoid the worst outcomes.
We can make things better; it’s not too late. But we
have to be willing to act.
Let’s start with the bad news. The Imperial College
response team’s report looked at the impact of measures we
might take to flatten the curve, or reduce the rate at which people are
becoming sick with COVID-19. If we do nothing and just let the virus run its
course, the team predicts, we could see three times as many deaths as we
see from cardiovascular disease each year.
Further, it estimated that infections would peak in mid-June. We could expect
to see about 55,000 deaths, in just one day.
Of course, we are doing something, so this outcome is
unlikely to occur. We’re closing schools and businesses and
committing to social (really, physical) distancing. But as the
sobering charts from the analysis show, this isn’t enough. Even after we do
these things, the report predicts that a significant number of infections will
occur, that more people will need care than we can possibly provide in our
hospitals, and that more than 1 million could die.
Why does the Imperial College team predict this for
the West when things seem to be improving in Asia? Because we are taking
different approaches. Asian countries have engaged in
suppression; we are only engaging in mitigation.
Suppression refers to a campaign to reduce the
infectivity of a pandemic, what experts call R0 (R-naught), to less than one.
Unchecked, the R0 of COVID-19 is between 2 and 3, meaning that every infected
person infects, on average, two to three others. An R0 less than 1 indicates
that each infected person results in fewer than one new infection. When this
happens, the outbreak will slowly grind to a halt.
To achieve this, we need to test many, many people,
even those without symptoms. Testing will allow us to isolate the infected so
they can’t infect others. We need to be vigilant, and willing to quarantine
people with absolute diligence.
Because we failed to set up a testing infrastructure, we
can’t check that many people. At the moment, we can’t even test everyone who is
sick. Therefore, we’re attempting mitigation—accepting that the epidemic will
advance but trying to reduce R0 as much as possible.
Our primary approach is social distancing—asking people to stay away
from one another. This has meant closing schools, restaurants, and bars. It’s
meant asking people to work from home and not meet in groups of 10 or more. Our
efforts are good, temporizing measures. Impeding the growth of the infection
improves the chance our health-care system will be able to keep up.
But these efforts won’t help those who are already infected. It will take up
to two weeks for those infected today to show any symptoms, and some people
won’t show symptoms at all. Social distancing cannot prevent these infections,
as they’ve already happened. Therefore, things will appear to get worse for
some time, even if what we’re doing is making things better in the long run.
The outbreak will continue to progress.
But buried in the Imperial College report is reason
for optimism. The analysis finds that in the do-nothing scenario, many people
die and die quickly. With serious mitigation, though, many of the measures
we’re taking now slow things down. By the summer, the report
calculates, the number of people who become sick will eventually reduce to a
trickle.
On this path, though, the real horror show will begin
in the fall and crush us next winter, when COVID-19 comes back with a
vengeance.
This is what happened with the flu in 1918. The spring was bad. Over
the summer, the numbers of sick dwindled and created a false sense of security.
Then, all hell broke loose. In late 1918, tens of millions of people died.
If
a similar pattern holds for COVID-19, then while things are bad now, it may be
nothing compared to what we face at the end of the year.
Because of this, some are now declaring that we might
be on lockdown for the next 18 months. They see no
alternative. If we go back to normal, they argue, the virus will run unchecked
and tear through Americans in the fall and winter, infecting 40 to 70 percent
of us, killing millions and sending tens of millions to the hospital. To
prevent that, they suggest we keep the world shut down, which would destroy the
economy and the fabric of society.
But all of that assumes that we can’t change, that the
only two choices are millions of deaths or a wrecked society.
That’s not true. We can create a third path. We can
decide to meet this challenge head-on. It is absolutely within our capacity to
do so. We could develop tests that are fast, reliable, and ubiquitous. If we
screen everyone, and do so regularly, we can let most people return to a more
normal life. We can reopen schools and places where people gather. If we can be
assured that the people who congregate aren’t infectious, they can socialize.
We can build health-care facilities that do rapid
screening and care for people who are infected, apart from those who are not.
This will prevent transmission from one sick person to another in hospitals and
other health-care facilities. We can even commit to housing infected people
apart from their healthy family members, to prevent transmission in households.
These steps alone still won’t be enough.
We will need to massively strengthen our medical
infrastructure. We will need to build ventilators and add hospital beds. We will
need to train and redistribute physicians, nurses, and respiratory therapists
to where they are most needed. We will need to focus our factories on turning out the protective equipment—masks,
gloves, gowns, and so forth—to ensure we keep our health-care workforce safe.
And, most importantly, we need to pour vast sums of intellectual and financial
resources into developing a vaccine that would finally bring this nightmare to
a close. An effective vaccine would end the pandemic and protect billions of
people around the world.
All of the difficult actions we are taking now to
flatten the curve aren’t just intended to slow the rate of infection to levels the
health-care system can manage. They’re also meant to buy us time. They give us
the space to create what we need to make a real difference.
Of
course, it all depends on what we do with that time. The mood of the country
has shifted in the last few weeks, from dismissal to one of fear and concern.
That’s appropriate. This is a serious pandemic, and it’s still very likely that
the rate of infection will overwhelm the surge capacity in some areas of the
United States. There will likely be more seriously ill people than we have
resources to care for, meaning that providers will have to make decisions about
whom to treat, and whom not to.
They may, explicitly or implicitly, have to decide who
lives and who dies.
If we commit to social distancing, however, at some
point in the next few months the rate of spread will slow. We’ll be able to
catch our breath. We’ll be able to ease restrictions, as some early hit
countries are doing. We can move toward some semblance of normalcy.
The temptation then will be to think we have made it
past the worst. We cannot give in to that temptation. That will be the time to
redouble our efforts. We will need to prepare for the coming storm. We’ll need
to build up our stockpiles, create strategies, and get ready.
If we choose the third course, when fall arrives, we
will be ahead of a resurgence of the infection. We can keep the number of those
who are exposed to a minimum, focusing our attention on those who are infected,
and enacting more stringent physical distancing only when, and in locations where,
that fails. We can keep schools and businesses open as much as possible,
closing them quickly when suppression fails, then opening them back up again
once the infected are identified and isolated. Instead of playing defense, we
could play more offense.
We need to keep time on the clock, time to find a
treatment or a vaccine.
The last time we faced a pandemic with this level of
infectivity, that was this dangerous, for which we had no therapy or vaccine,
was a 100 years ago, and it led to 50 million deaths. The coronavirus pandemic
isn’t unprecedented, but it’s not anything almost anyone alive has experienced
before. We, are, however, much more knowledgeable, much more coordinated, and
much more capable today.
Some Americans are in denial, and others are feeling
despair. Both sentiments are understandable. We all have a choice to make. We
can look at the coming fire and let it burn. We can hunker down, and hope to
wait it out—or we can work together to get through it with as little damage as
possible. This country has faced massive threats before and risen to the
challenge; we can do it again. We just need to decide to make it happen.